Precision Medicine and Genomics: Revolutionizing Organ Transplants
Medical science is advancing at an unprecedented rate, and one of the most promising areas of progress is precision medicine and genomics. Precision medicine, which involves tailoring healthcare treatments to individual patients based on their genetic information, is transforming the landscape of modern medicine. One field that stands to benefit immensely from these advancements is organ transplantation. By leveraging precision medicine and genomics, healthcare providers can improve the success rates of organ transplants, minimize complications, and enhance the overall quality of life for patients. In this article, we will explore how precision medicine and genomics are revolutionizing organ transplants, the challenges involved, and the future of this transformative field.
Understanding Precision Medicine and Genomics
Precision medicine is a medical approach that considers individual variability in genes, environment, and lifestyle when diagnosing and treating patients. Genomics, a key component of precision medicine, involves the study of an individual’s complete set of DNA, including all of their genes. By understanding the genetic makeup of both the donor and the recipient, healthcare professionals can make more informed decisions about organ compatibility, post-transplant treatments, and individualized patient care.
1. What Is Precision Medicine?
Precision medicine involves using detailed information about a patient’s genetic makeup, environment, and lifestyle to develop personalized treatment plans. Unlike traditional medicine, which often uses a “one-size-fits-all” approach, precision medicine aims to tailor treatments to meet the unique needs of each individual.
- Targeted Treatment: Precision medicine enables healthcare providers to identify which treatments are most likely to work for a specific patient, reducing the need for trial and error.
- Prevention Focus: By understanding genetic predispositions, precision medicine can also be used for disease prevention and early intervention, helping patients make informed decisions about their health.
2. What Is Genomics?
Genomics is the study of the entire set of genes (genome) of an organism. In the context of precision medicine, genomics provides valuable insights into how genetic variations can impact an individual’s response to different medical treatments.
- Genetic Sequencing: By sequencing a patient’s genome, healthcare providers can identify mutations or variations that may affect organ transplant outcomes.
- Understanding Compatibility: Genomics helps determine compatibility between donors and recipients, reducing the risk of organ rejection and improving the likelihood of a successful transplant.
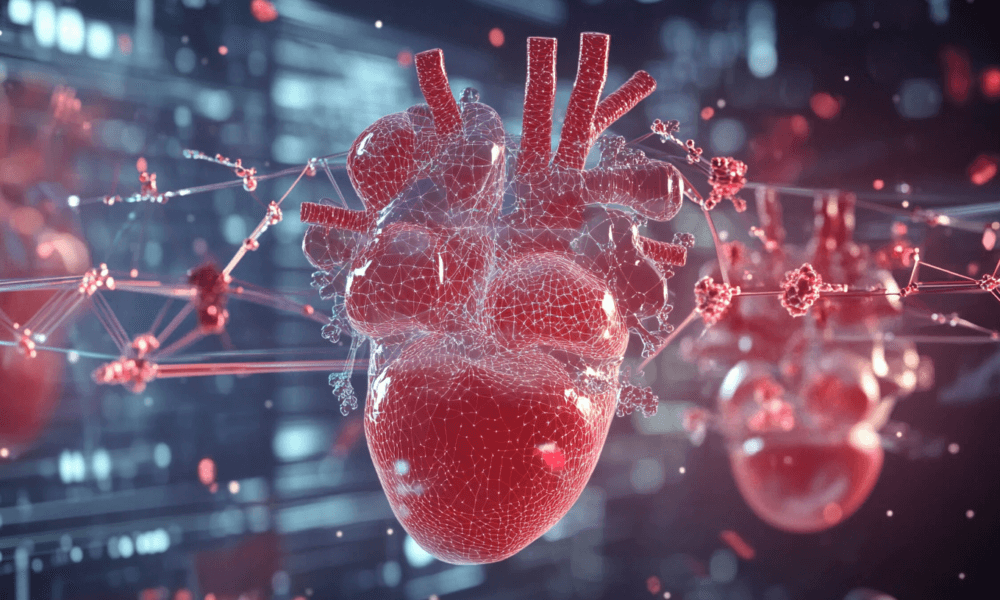
The Role of Precision Medicine in Organ Transplants
Organ transplantation is a life-saving procedure for patients with end-stage organ failure. However, the success of transplants is often hindered by complications such as organ rejection and the need for lifelong immunosuppressive drugs. Precision medicine and genomics have the potential to address these challenges and improve the entire transplant process.
1. Improving Donor-Recipient Matching
The success of an organ transplant depends largely on the compatibility between the donor and the recipient. Traditionally, donor-recipient matching has relied on factors such as blood type and human leukocyte antigen (HLA) compatibility. Precision medicine and genomics take this process a step further by analyzing the genetic makeup of both the donor and the recipient to ensure a better match.
- Genetic Profiling: By conducting a comprehensive genetic analysis of both parties, doctors can identify potential incompatibilities and assess the likelihood of rejection before the transplant.
- Reducing Rejection Rates: Genomic data can help predict the immune response of the recipient, enabling healthcare providers to choose a donor organ with the highest chance of success and minimize rejection.
2. Personalized Immunosuppressive Therapy
One of the biggest challenges in organ transplantation is the need for immunosuppressive drugs to prevent rejection. These drugs can have significant side effects and may not work equally well for all patients. Precision medicine can optimize immunosuppressive therapy by tailoring it to the specific genetic profile of the recipient.
- Tailored Dosage: By understanding how a patient’s genes influence drug metabolism, doctors can determine the most effective dosage of immunosuppressive drugs, reducing side effects and improving the patient’s quality of life.
- Minimizing Complications: Genomic insights can also help identify patients who are at a higher risk of adverse reactions to certain drugs, allowing doctors to select alternative medications or adjust the treatment plan accordingly.
3. Early Detection of Organ Rejection
Organ rejection remains a significant risk following a transplant, and early detection is crucial for effective intervention. Genomics and precision medicine can aid in the early identification of rejection, even before symptoms become apparent.
- Biomarker Identification: Genomic analysis can identify biomarkers that indicate early signs of rejection, allowing doctors to intervene before irreversible damage occurs.
- Non-Invasive Monitoring: Liquid biopsies, which involve analyzing a patient’s blood for genetic markers, provide a non-invasive method for monitoring transplant health and detecting rejection at an early stage.
Genomics and the Future of Organ Transplants
The integration of genomics into organ transplantation is opening new possibilities for improving patient outcomes and expanding the availability of donor organs. Here are some of the ways genomics is shaping the future of organ transplants:
1. Xenotransplantation
Xenotransplantation, the transplantation of organs from animals to humans, has the potential to address the shortage of human donor organs. Genomics is playing a critical role in making xenotransplantation a viable option.
- Genetic Modification: By using gene-editing tools like CRISPR, scientists can modify the genes of animals (such as pigs) to make their organs more compatible with the human immune system, reducing the risk of rejection.
- Overcoming Immunological Barriers: Genomics can help identify and modify specific genes that trigger immune responses, making xenotransplantation safer and more feasible.
2. 3D Bioprinting and Regenerative Medicine
Advances in regenerative medicine and 3D bioprinting are being combined with genomics to create customized organs for transplantation. This approach has the potential to eliminate the need for donor organs altogether.
- Bioprinted Organs: By using a patient’s own cells and genomic data, scientists can create bioprinted organs that are genetically identical to the recipient, eliminating the risk of rejection.
- Personalized Regenerative Therapy: Genomics can also aid in regenerative therapies, where damaged organs are repaired using stem cells that are genetically modified to match the patient’s needs.
3. Expanding the Donor Pool
The shortage of donor organs is a major challenge in organ transplantation. Genomics is helping to expand the donor pool by making previously incompatible organs viable for transplantation.
- Genetic Desensitization: Genomic techniques can be used to modify the immune system of recipients, making them more tolerant of donor organs that would otherwise be incompatible.
- Optimizing Marginal Donor Organs: Genomic analysis can help determine which marginal donor organs—those that are initially deemed unsuitable—can be safely used for transplantation, thereby increasing the number of available organs.
Challenges and Ethical Considerations
While the advancements in precision medicine and genomics are promising, there are also several challenges and ethical considerations that need to be addressed to ensure the successful integration of these technologies in organ transplantation.
1. Cost and Accessibility
Precision medicine and genomic sequencing can be expensive, making it challenging for many patients to access these advanced treatments.
- High Costs: The cost of genomic testing and personalized treatment plans can be prohibitive, limiting access for patients in lower-income communities or countries.
- Insurance Coverage: There is also the question of whether insurance companies will cover the costs associated with genomic testing and precision medicine, which could impact its widespread adoption.
2. Data Privacy and Security
Genomic data contains highly sensitive information, and protecting patient privacy is a critical concern.
- Data Security: Ensuring the security of genomic data is crucial to prevent unauthorized access and misuse of personal information.
- Informed Consent: Patients need to be fully informed about how their genetic data will be used, stored, and shared. Informed consent is essential to maintain trust and ethical standards in medical research and treatment.
3. Ethical Concerns in Gene Editing
Gene editing, particularly in the context of xenotransplantation and organ modification, raises ethical questions.
- Animal Rights: The use of animals for organ transplantation raises concerns about animal welfare and the ethical implications of genetic modification.
- Unintended Consequences: Gene editing is still a relatively new technology, and there is a risk of unintended consequences or off-target effects that could impact both donors and recipients.
Conclusion
Precision medicine and genomics are revolutionizing the field of organ transplantation by improving donor-recipient matching, personalizing immunosuppressive therapy, and enabling early detection of rejection. Advances in genomics are also paving the way for innovative approaches such as xenotransplantation, 3D bioprinting, and regenerative medicine, which could address the shortage of donor organs and improve transplant outcomes. However, challenges related to cost, accessibility, and ethical considerations must be addressed to ensure that these life-saving technologies are available to all who need them. By investing in research, developing ethical frameworks, and ensuring equitable access, we can unlock the full potential of precision medicine and genomics, ultimately transforming the future of organ transplantation and saving countless lives.


No Comment! Be the first one.